Aged Care Services

We care about our aging community and their quality of life!
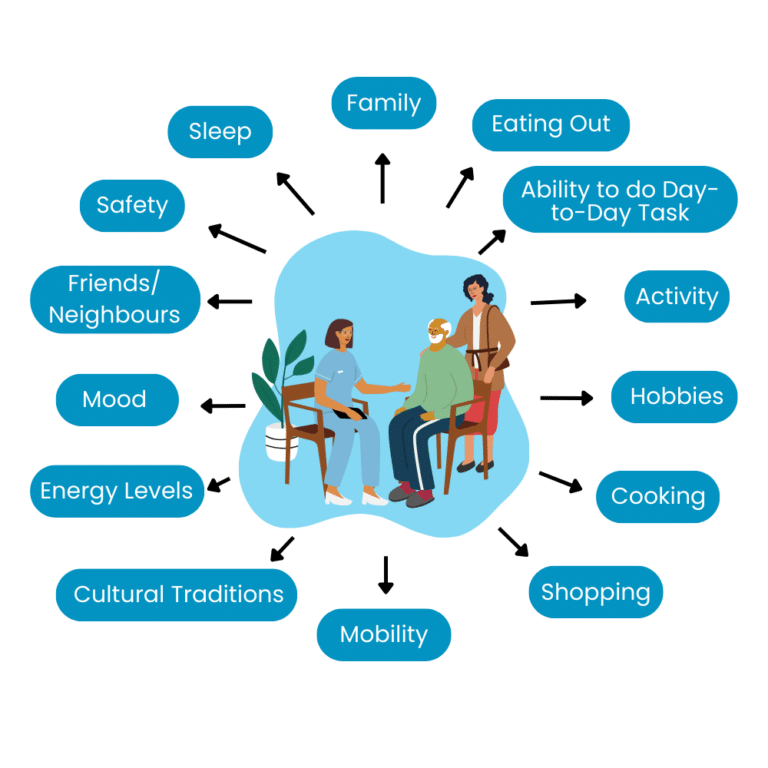
We centre our care around each human being as they are, to make the experience and end goal more than just meeting nutritional requirements.
How We Can Help
Everyone should have the opportunity to stay in their home for as long as possible. Our dietitians will help you stay healthy, allowing you to make this goal a reality and live a fulfilling and independent life.
We are the experts in the field, having provided over
100,000
Home Visit Consults
We’re Everywhere!
We are the largest dietetic company in Australia and have 45+ dietitians with extensive experience, spread across most major geographical regions. Chances are, we are, where you are!
What Funding is Available?
The Government Home Care Package funded program can allow you to see one of our dietitians. Get started immediately if you are with one of our current home care providers.




With a Different Home Care Provider?
We work with many providers, let us know your provider in our enquiry form below and we will get in touch to see if we can work together for you to access our dietitians.
What We Commonly Help Our Aging Community With
Unintentional Weight Loss
– Restore normal body weight
Loss of Appetite
– Strategies and advice to improve appetite and prevent weight loss and nutritional deficiency
Loss of Muscle Mass
– Support food access and appropriate food choices to prevent weight loss
Frequent Illness/Hospitalisation Prevention
– Support recovery after a period of compromised nutrition and address increased nutritional needs during recovery.
Recent Fall
– Strategies to support home food environment to prevent fall, hospitalisations and illness.
Change in Social/Living Situation (eg Loss of a partner or partner moved into high care, Family/supports changed or seeking meal delivery service)
– Education and support with nutritional strategies to ensure maintaining healthy diet and weight.
– Nutrition based counselling, with support for increased skills, and strategies to enable improved cooking abilities and assistance in re-engagement of cooking duties.
– Guidance with choosing frozen meals or meal delivery services that will cater to individual needs
Low Body Weight
– Strategies and education to nutritiously increase oral intake to support weight gain and overall health.
– Supporting food access, appropriate food choices and meal regularity to facilitate increase in weight.
Cognitive or Functional Decline
– Education and support with nutritional strategies to ensure maintaining healthy diet and weight.
– Conversation surrounding the importance of diet quality and how this can relate to dementia/Alzheimer’s progression.
– Education and support on nutritional considerations and prioritisation changes over time associated with cognitive decline.
– Guidance with choosing frozen meals or meal delivery services that will cater to individual need
Poorly Healing or Frequent Wounds
– Education surrounding the importance of nutritional adequacy to assist with the healing of wounds.
– Manipulation of diet to help assist in improved healing (ensuring appropriate intake of carbohydrates, protein and energy) based on individuals daily needs.
Weight Loss Goals
– Individualised strategies to assist with weight management to improve quality of life.
– Strategies and education to improve food choices, facilitate energy deficit and reduction in body weight.
– Address and account for possible existing comorbidities and prevent progression of chronic disease.
Diabetes
– Education on diet disease relationship to assist with understanding on diet modification.
– Medical Nutrition therapy to assist reduce progression of disease (including altering carbohydrates, protein, sodium, saturated fat, potassium, and phosphate, etc. as relevant).
– Education and prescription of anti-inflammatory diet principles.
– Individualised strategies to assist with weight management to reduce pain and improve mobility
Chronic Kidney Disease
– Education on diet disease relationship to assist with understanding on diet modification.
– Medical Nutrition therapy to assist reduce progression of disease (including altering carbohydrates, protein, sodium, saturated fat, potassium, and phosphate, etc. as relevant).
– Education and prescription of anti-inflammatory diet principles.
– Individualised strategies to assist with weight management to reduce pain and improve mobility
Cardiovascular/Heart Disease (previous heart attack/stroke, high cholesterol, hypertension, stents/valve replacements, etc.)
– Education on diet disease relationship to assist with understanding on diet modification.
– Medical Nutrition therapy to assist reduce progression of disease (including altering carbohydrates, protein, sodium, saturated fat, potassium, and phosphate, etc. as relevant).
– Education and prescription of anti-inflammatory diet principles.
– Individualised strategies to assist with weight management to reduce pain and improve mobility
Gastrointestinal Issues (eg. constipation / Diarrhoea, reflux, Change in bowel habits, Inflammatory bowel disease, Excessive belching or gas, abdominal pain, Diverticular Disease, IBS)
– Assistance regarding diet modification to relieve symptoms (includes, but not limited to manipulation of fibre, fluid, sugar, fat, caffeine and alcohol intake).
– Implementation of toilet regime to assist with healthy bowel movements.
– Conversation regarding laxatives/ anti-diarrheal as seen appropriate.
– Individualised medical nutrition therapy regarding GI condition/s, based on diagnosis and symptoms.
Anaemia or Iron Deficiency
– Education regarding the importance of macronutrients/ micronutrients play in specific condition/s.
– Ensuring nutritional adequacy through foods within diet to meet micronutrient needs.
– Implementation of dietary supplementation for lacking micronutrients, if seen fit.
Osteopenia or Osteoporosis
– Education regarding the importance of macronutrients/ micronutrients play in specific condition/s.
– Ensuring nutritional adequacy through foods within diet to meet micronutrient needs.
– Implementation of dietary supplementation for lacking micronutrients, if seen fit
Vegetarian/Vegan Diets
– Education regarding the importance of macronutrients/ micronutrients play in specific condition/s.
– Ensuring nutritional adequacy through foods within diet to meet micronutrient needs.
– Implementation of dietary supplementation for lacking micronutrients, if seen fit
Vegetarian/Vegan Diets
– Education regarding the importance of macronutrients/ micronutrients play in specific condition/s.
– Ensuring nutritional adequacy through foods within diet to meet micronutrient needs.
– Implementation of dietary supplementation for lacking micronutrients, if seen fit
Poor Mental Health
– Education and prescription of anti-inflammatory diet principles, and how this has been shown to improve mental health.
– Ensuring meeting adequate nutrients to assist with improved mental health through dietary change, with additional focus on enjoyment of foods

